The DANGERS of Antibiotic Resistance
November 26, 2012
Every day we hear reports of new strains of deadly viruses, bacteria and fungal infections that claims the lives of unsuspecting people all over the world. And researchers, scientists, healthcare providers with the help of government and pharmaceutical companies all scramble against time to find the most effective cure. But before these "miracle" drugs really go for mass production for human consumption, patients have to wait for years of animal and human trials and post marketing surveillance for drug side effects before a new drug can be certified safe for human use. Sir Alexander Fleming was awarded a Nobel prize for his discovery of the drug penicillin in 1928 but took the world 12 years to mass produce it in 1941, just in time to treat infections in injured soldiers during the Second world war.
Antibiotics are our most important tools to combat bacterial infections that have been proven time and time again to save lives from serious to life threatening diseases caused by living microorganisms we call bacteria. To the clinician, it is one part of his armamentarium to treat infections that are found to be BACTERIAL in nature. Over the last 2 to 3 decades, as the medical profession became more technologically advanced, it has also revolutionized the way we understand bacterial infections, from the vast array of mechanisms they use to get inside our bodies, from the toxins and chemicals they produce to create the signs and symptoms that we usually face in the clinics, and even up to the mechanisms on how they are able to evade our immune responses-- all of these knowledge with the help of medical science has made our patients live longer and enjoy a better quality of life compared to humanbeings who lived 50 to 100 years ago.
But during the last 2 to 3 decades, antibiotic resistance or the ability of bacteria to bypass the effects of antibacterial medications has led to one of the worlds' most pressing public health threats according to the Centers of Disease Control (CDC), and the main culprit is the inappropriate use of antibiotics by clinicians who prescribe it without any basis or regards to its potential side effects to their patients, not to mention it creates a huge economic burden to the entire healthcare system of a country where, financial difficulty is faced by most of its citizens for the main reason that they are harder to treat and requires longer hospital stays. Of which, we as clinicians prescribing this medications should carefully ponder about.
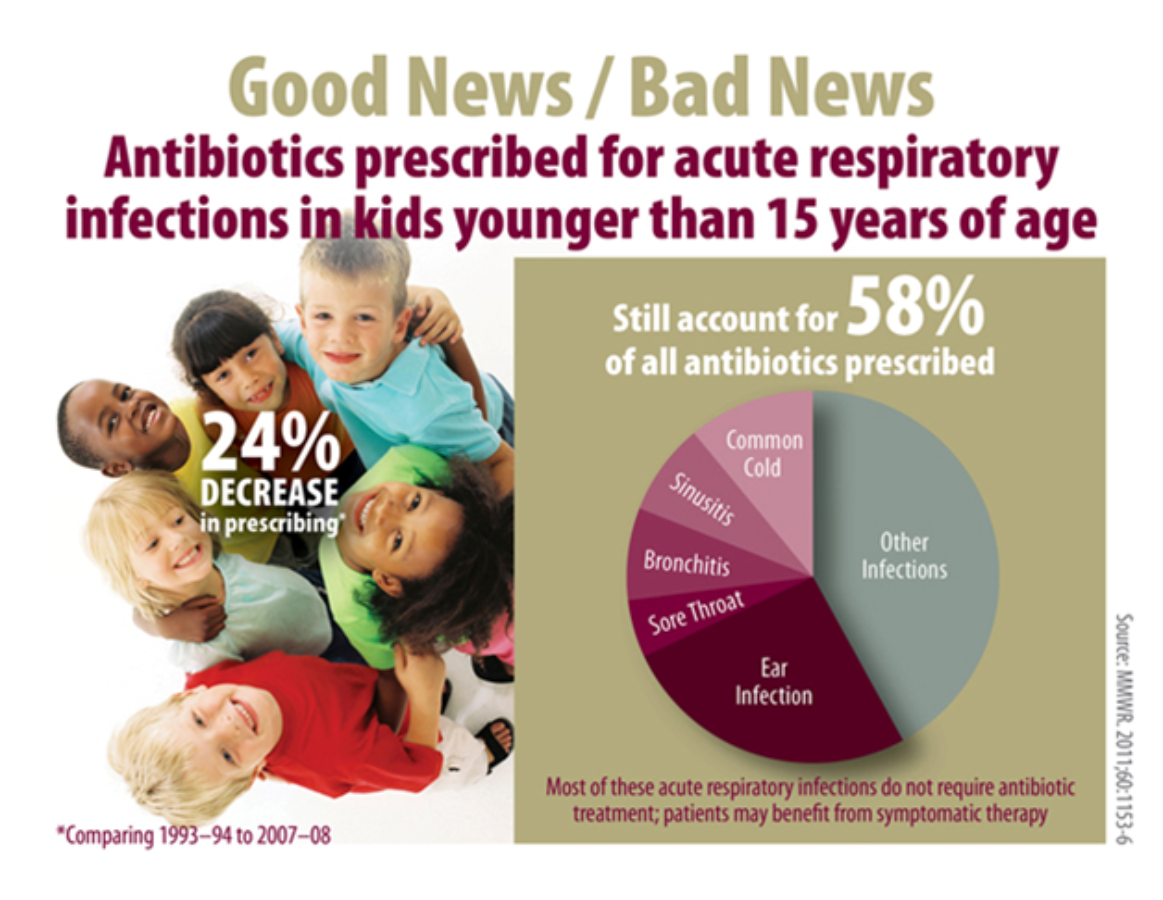
According to the Journal of the American Medical Association (JAMA, Aug.2009) issue regarding the use of antibiotics in respiratory illnesses, infections which can be easily treated without the need for antibiotics are, the common cold, influenza(flu), most coughs and bronchitis, many ear infections including otitis media and many skin rashes. It recommends clinicians to be more SMART and strictly adhere to these guidelines in treating this kinds of conditions when patients' presents to their clinics to help prevent emergence of resistant strains and maintains that home rest, lots of fluids and symptomatic relief medications is all it takes to do the job.
The emergence of Methicillin Resistant Staphylococcus aureus(MRSA), Drug resistant Streptococcus pneumoniae that causes severe pneumonia, meningitis and blood infections (Septicemia) and Multiple Drug Resistant Tuberculosis (MDRTB) are only a few of the many antibiotic resistant bacteria that doctors and hospitals are facing all around the world everyday--which is largely due to inappropriate use of antibiotics by primary care providers at the outset. Aside from giving right medications to patients, doctors at the outpatient clinic, whether public or private has the duty to inform their patients about the drugs that they are prescribing, its rationale and potential side effects, as well as to educate their patients that it doesn’t mean that if the doctor is not giving an antibiotic, it doesn’t mean that they aren’t sick, BUT clinicians need to explain that prescribing antibiotics inappropriately will NOT help cure the infection, will NOT keep other people from getting sick, will NOT help the patient feel any better and may only cause unnecessary and unwanted side effects.
I call on patients, colleagues in the healthcare sector, hospital administrators and including policy makers to join and work together to design an effective and safe strategy to improve antibiotic use that will ultimately -save human lives.

Comments
No comments