We are in the sickness business: we need to get into the health business
– Shinah, COO –
In an article in Time magazine a doctor had commented that he never saw a patient who was well, all his time as a heart surgeon, all he saw was patients who were sick. Some might argue that why should someone who is in good health go to see a Dr especially in Maldives. It’s hard to get an appointment for a Dr and even more difficult and time consuming to actually see the Dr, do the test or x rays. The health system in this country as well as other countries is designed to treat sickness and disease care rather than health care. Clinics and hospitals are more focused on curing the sick than actually trying to prevent the sickness and advocating for healthy lifestyles. Hardly there are clinics, programs, seminars, lectures or even consultation sessions that are designed for healthy living and staying healthy by the local health care providers. With the introduction of National health insurance in the Maldives, people are ever more discouraged to visit Dr’s when they are healthy which is rightly so as it increases the burden on the insurance scheme.
 Cleveland Clinic a 1100 bedded Hospital in Cleveland, USA has adopted a new view of health care, where Physicians, Patients and Staff of the hospital are enrolled in a program called “Lifestyle 180” which is an innovative approach to good health that uses cooking classes, exercise sessions, counselling and yoga to educate patients about how to eat better, become more physically active, manage stress and, ultimately prevent long term and chronic illnesses such as heart attack, cholesterol, diabetes and strokes. The participants are given a tool kit, complete with yoga mat, recipe book and tips on navigating the food aisles in super markets, which is part of being health conscious, and assist in living a healthy life. In Addition to the hospital other corporations and business sponsor people to join this program to encourage people to start living healthily.
Cleveland Clinic a 1100 bedded Hospital in Cleveland, USA has adopted a new view of health care, where Physicians, Patients and Staff of the hospital are enrolled in a program called “Lifestyle 180” which is an innovative approach to good health that uses cooking classes, exercise sessions, counselling and yoga to educate patients about how to eat better, become more physically active, manage stress and, ultimately prevent long term and chronic illnesses such as heart attack, cholesterol, diabetes and strokes. The participants are given a tool kit, complete with yoga mat, recipe book and tips on navigating the food aisles in super markets, which is part of being health conscious, and assist in living a healthy life. In Addition to the hospital other corporations and business sponsor people to join this program to encourage people to start living healthily.
With health care and medicines costing more and more each day as well as the emotional trauma of having long illnesses or taking care of sick people, this approach of health care is something that we need to adopt in the Maldives. Especially with the social difficulties that are part and parcel of living in Male, few people would want to get a long term sickness and be confined to hospital much worse at home where most of the population lives in small concrete blocks. In the islands where there are more spacious living conditions and less stress compared to Male’ the healthcare is not at the same standard.
While prevention is very much talked about by the medical profession it has never been practiced as it should be, while government, politicians, health care providers are talking about the increase in the cost of health care, few realize that spending in preventive, healthy life style programs and educating the public will in the long term reduce the cost of health care, as more people will adopt better living philosophies which in turn will make people less sick. The insurance companies should cover to some extent these sorts of preventive health programs, clinics and consultations so as to encourage more people to be healthy. Corporations should endorse such programs in to the corporate structure and help the employees in being healthy. Most of all hospitals and clinics and Dr’s should start programs that are designed to make the population healthy and prevent sicknesses.
World Sickle Cell Day
Mohamed Akram-Abdulla MBBS, MRCP (UK) [Maldives Medical Association Contribution]
A United Nations resolution made 19th June as World Sickle Cell Day (WSCD). Globally there are probably over 2 million people who are affected with the disease. Though I have no statistical evidence, it is likely that a number of individuals in the Maldives are affected by this painful, life shortening illness. This disease not only carries a high morbidity and mortality with it but also the emotional and financial burden is huge. As health professionals it is incumbent upon us to make sure we support these individuals as best as we can. The least, perhaps, we could do for them is making sure we diagnose them early and correctly, offer the right treatment and provide them the right information. The aim of the summary review below is to increase awareness among the medical community about the condition and the specific therapies that are available today. It is not possible to cover all aspects of the disease however I hope it gives some insight regarding this gruesome disease.
Sickle cell disease (SCD)
Background
Sickle cell disease (SCD) and its variants are genetic disorders. It is an autosomal recessive disorder first described by Herrick in 1910. This occurs due to a mutation in the Haemoglobin, called Haemoglobin S (HbS). SCD causes significant morbidity and mortality, particularly in people of African and Mediterranean ancestry. Morbidity, frequency of crisis, degree of anemia, and the organ systems involved vary considerably from individual to individual. The most common form of the disease is the HbSS variant. This essentially means the individual has tow abnormal haemoglobins which then leads to precipitation of the disease. Though almost all suffer from various degrees of clinical symptoms the severity of the symptoms vary hugely form individual to individual and at times can be a diagnostic challenge specially in places where medical facilities and diagnostics are readily not available. Almost half of the individuals with the homozygous status of the disease experience vaso-occlusive crisis. But the frequency and the severity of the crisis again vary from individual to individual. Some have more 6 o more such events a year while some may have a few or none. Most people with HbSS suffer from low level chronic pain mainly in the bones and in some individuals this may be the only presenting symptoms of the disease. A crisis may present as worsening of this pain.
A person is said to be a carrier when the individual has an HbS along with normal adult hemoglobin (HbA). These individuals usually do not manifest clinical symptoms. However when an HbS is mixed with another form of abnormal hemoglobin then they may suffer from milder form of the disease on one such example is when HbS is mixed with beta-thalassemia, known as sickle beta thalassemia.
Epidemiology
The disease is found worldwide but prevalence of the trait is as high as 30% in several parts of Africa. It is also found in some parts of Sicily, Greece, Turkey and India. The mutation that results in HbS is believed to have originated from India and Africa. This is perhaps due to the survival advantage that the heterozygote forms offer against plasmodium falciparum, a form of Malaria. I have no doubt the disease exist in the Maldives though we are short of any statistical figures.
Disease characteristics at various ages
Haematological abnormalities can be noted as early as 10 weeks but clinical manifestation often do not occur until later part of the first year when the fetal Hb decline and this allows the abnormal HbS to cause clinical symptoms. SCD disease then persist life long though it is believed that the painful crisis decrease after 10 years but complication rate increases thereafter. The mean age patients with SCD develop end-satge renal disease is about 23 years and median life expectancy even with dialysis is about 27 years.
How do patients with SCD present.
General Overview — The clinical manifestations of sickle cell disease vary markedly among the major genotypes. The term sickle cell disease s generally used to describe all of the conditions associated with the phenomenon of sickling, whereas the term sickle cell anaemia is generally used to describe homozygosity for haemoglobin S (ie, Hb SS). The disorder is most severe in patients with homozygosity for HbS. Among patients with sickle cell-beta thalassemia, the disease varies with the quantity of hemoglobin A, often being quite severe in patients with sickle cell-beta (0) thalassemia and less severe in patients with sickle cell-beta (+) thalassemia. It is best to describe the manifestations of the disease under the following sub headings.
Chronic pain in SCD
Many individuals with SCD experience chronic low-level pain, mainly in bones and joints. Intermittent vaso-occlusive crises may be superimposed, or chronic low-level pain may be the only expression of the disease.
Anaemia
This is a universal feature. In the right context if a child is found to be anaemic the possibility of SCD or one of its variants such as sickle cell beta thalassemia should be explored. Most tolerate the anaemia very well and are not symptomatic with daily activities of living but the gie away would their low tolerance to exertions compared to their healthy peers.
Aplastic crisis
A serious complication s caused by infection with Parvovirus B-19 (B19V). This virus causes fifth disease, a normally benign childhood disorder associated with fever, malaise, and a mild rash. This virus infects the RBC precursors and can cause an acute drop in haemoglobin in patients with SCD.
Splenic sequestration
This condition occurs when spleen destroys the abno ormal RBC at a very rapid rate and causes very acute drop in Hb. This also results in progressive splenomegaly. This is a medical emergency requiring transfusion support, close monitoring and often splenectomy in older children.
Infection
Organisms that pose the greatest danger include encapsulated respiratory bacteria, particularly streptococcus pneumonia. The mortality rate of such infections has been reported to be as high as 10-30%. Consider osteomelitis when dealing with a combination of persistent pain and fever. Bone that is involved with infarct-related vaso-occlusive pain is prone to infection. Staphylococcus and Salmonella are the 2 most likely organisms responsible for osteomyelitis.
During adult life, infections with gram-negative organisms, especially Salmonella, predominate. Of special concern is the frequent occurrence of Salmonella osteomyelitis in areas of bone weakened by infarction.
Effects on growth and maturation
During childhood and adolescence, SCD is associated with growth retardation, delayed sexual maturation, and being underweight. Growth delays during puberty in adolescents with SCD are independently associated with decreased Hb concentration and increased total energy expenditure.
Hand-foot syndrome
The syndrome develops suddenly and lasts 1-2 weeks. Hand-foot syndrome occurs between age 6 months and 3 years; it is not seen after age 5 years. This is a dactiliytis and presents with severe pain along with swelling of dorsum of hands and feet.
Acute chest syndrome
Acute chest syndrome is a medical emergency and must be treated immediately. This carries significant risk of acute respiratory distress syndrome. Acute chest syndrome probably begins with infarction of ribs, leading to chest splinting and atelectasis. Because the appearance of radiographic changes may be delayed, the diagnosis may not be recognized immediately. Other conditions to think of are pulmonary infarction and fat embolism resulting from bone marrow infarction.
Central nervous system involvement
Central nervous system involvement is one of the most devastating aspects of SCD. Stroke affects 30% of children and 11% of patients by 20 years. It is usually ischemic in children and hemorrhagic in adults. Hemiparesis is the usual presentation but may present with other defects. Convulsions are frequently associated with stroke. Hemorrhagic stroke is associated with a mortality rate of more than 29%.
Cardiac involvement
The heart is involved due to chronic anemia and microinfarcts. Haemolysis and blood transfusion lead to haemosiderin deposition in the myocardium. This significantly Increases the risk of dilated cardiomyopathy.
Renal involvement
The kidneys lose concentrating capacity. Isosthenuria results in a large loss of water, further contributing to dehydration in these patients. Renal failure may ensue, usually preceded by proteinuria.
Eye involvement
Proliferative retinitis is common in SCD and may present with loss of vision.
Leg ulcers
These are often chronic and painful. Circulation is poor and increases risk of infection
Priapism
Priapism, defined as a sustained, painful, and unwanted erection, is a well-recognized complication of SCD. Priapism tends to occur repeatedly. It may lead to impotence. Mean age at which priapism occurs is 12 years, and, by age 20 years, as many as 89% of males with SCD would have experienced one or more episodes of priapism. Priapism can be classified as prolonged if it lasts for more than 3 hours or as stuttering if it lasts for more than a few minutes but less than 3 hours and resolves spontaneously. Prolonged priapism is an emergency that requires urologic consultation.

Figure 2: Clinicopathologic findings in sickle cell anaemia. The findings are a consequence of infarctions, anaemia, haemolysis, and recurrent infection. From Damjanov, 2000. (Ref: http://medical-dictionary.thefreedictionary.com)
Pulmonary hypertension
Various studies have found that more than 40% of adults with SCD have pulmonary hypertension that worsens with age. This incidence is as high as 30%. This is associated with high mortality in adults.
Diagnosis of sickle cell syndrome
Prenatal Testing
The sickle haemoglobin diseases (ie, sickle cell anaemia, haemoglobin SC disease, sickle cell beta thalassemia) are chronic, debilitating and sometimes fatal. The severe clinical nature of these diseases, particularly SCD and sickle cell beta thalassemia, and the absence of curative therapy are the primary stimulants for the development of foetal sampling and DNA-based diagnostic methodology. Couples at risk should be offered haemoglobinopathy testing early in pregnancy and the opportunity for prenatal diagnosis where appropriate.
Newborn Screening
Infants with SCD generally are healthy at birth and develop symptoms only when foetal haemoglobin levels decline later in infancy or early childhood.
The goals of newborn screening are
- Early recognition of affected infants
- Early medical intervention to reduce morbidity and mortality, particularly from bacterial infections
- Institution of regular and ongoing comprehensive care through a multidisciplinary sickle cell clinic, in collaboration with the primary care physician, whenever feasible
- Access for families of children with SCD to accurate information about the diagnosis, clinical manifestations, treatment options, and age-appropriate anticipatory guidance toward the management of these emerging issues.
Older children and adults
The purpose of correct diagnosis in this age group is to identify patients who need therapy for sickle cell disease and counselling for the disease or the trait. Despite newborn screening, many patients with sickle cell disease may be undiagnosed, in part due to immigration of young, unscreened patients from other countries.
A brief look at blood abnormalities
Typical baseline abnormalities in the patient with SCD include
- Hemoglobin level is 5-9 g/dL
- Hematocrit 17-29%
- Total leukocyte count is elevated to 12,000-20,000 with a predominance of neutrophils
- Platelet count is increased
- ESR is low
- The reticulocyte count is usually elevated, but it may vary depending on the extent of baseline hemolysis
- Peripheral blood smears demonstrate target cells, elongated cells, and characteristic sickle erythrocytes
- Presence of RBCs containing nuclear remnants (Howell-Jolly bodies) indicates that the patient is asplenic

Figure 3: The HbS gene causes the red blood cells to become abnormally crescent-shaped and rigid, like sickles used to cut wheat. (Ref: understandingrace.org)
Results of hemoglobin solubility testing are positive, but they do not distinguish between sickle cell disease and sickle cell trait.
There are several other investigations that will need to be carried out during the complete work up but once the diagnosis is made it is important to tailor the investigations to answer most pressing clinical problem.
Specific therapies for Sickle cell disease
The only cure for the disease at present time is haematopoetic cell transplant (bone marrow transplant) and hydroxyurea is the only major medical modality with proven efficacy in patients with frequent symptoms related to SCD
Summary of treatment recommendation
Children and adults
In children older than two years of age and adults with sickle cell disease who have frequent painful episodes, severe symptomatic anemia, or a history of acute chest syndrome or other severe vasoocclusive events, treatment with hydroxyurea is recommended (evidence Grade 1A). This agent should be continued for as long as it is tolerated and effective.
Very young children
Very young children (ie, 9 to 18 months of age) with SCD, independent of disease severity, be treated with hydroxyurea . Compounding pharmacy support is required because a liquid form of the medication is not yet available. The evidence was recently downgraded from 1A recommendation to a 2A suggestion because of the lack of long-term safety data for children in this age range.
There is no information on the safety and efficacy of hydroxyurea in children younger than nine months of age. However, given the high prevalence of splenic damage prior to nine months of age, the use of hydroxyurea in children younger than nine months of age with symptomatic disease is recommended (The evidence is weak Grade 2C). In children who have been started on hydroxyurea in this age range who remain asymptomatic or minimally symptomatic, hydroxyurea should be continued indefinitely, (Evidence Grade 2B)
Children and adults with minimal disease activity — In adults and children who are older than 18 months of age and who have been asymptomatic or minimally symptomatic without treatment with hydroxyurea, should not be started (Evidence Grade 2C).
Data are sparse concerning its benefit, however addition of erythropoietin in patients not responding to hydroxyurea alone is often standard practice (Evidence Grade 2C).
Transfusion with packed red blood cells should be given when symptomatic anaemia is present.
Monitoring
During treatment with hydroxyurea patients should have regular FBC, with red cell indices, white blood cell differentials, reticulocyte percentage. Renal and liver function should be monitored regularly. Childbearing age females should have a pregnancy test before starting the medication and appropriate contraceptive advice should be offered.
Transplantation — Indications for marrow transplantation in patients with sickle cell disease have included the presence of severe debilitating clinical events such as stroke, recurrent acute chest syndrome, and recurrent painful vaso-occlusive crises. This procedure, which can be associated with considerable morbidity and mortality, has been generally limited to children and young adults with an HLA-matched sibling donor.
Novel therapies
Gene Therapy — Although still experimental, gene therapy has the potential to cure SCD Expression of the human sickle gene in transgenic mice and creation of plasmids with the human beta globin locus are examples of the possible feasibility of this approach. This approach is believed to increase the foetal Hb and as we know high levels of foetal Hb prevents sickling.
Nicosan — The only one herbal agent tested to date, nicosan, has proved to have an efficacy/toxicity ratio sufficiently high to merit testing in clinical trials. Nicosan is a plant extract that has been successfully used in Nigeria to prevent painful crises associated with SCD .The exact mechanism of action, active ingredient(s), and long-term side effects are unknown, nicosan inhibits sickling in vitro as well as in vivo in a transgenic mouse model of SCD. Nicosan has been granted orphan drug status by the United States FDA and the European Medicine Evaluation Agency, but there is no commercial supplier of the agent.
Acute pain plan
Every adult with sickle cell disease (SCD) should have an established pain plan tailored to his/her individual needs. This plan should instruct the individual how to appropriately manage mild, moderate, and severe pain, with a pre-defined threshold for the use of opioids and when to contact health care providers. Optimally, an individualized pain plan has been established in the ED with the haematology team.
Pain management in the A&E
For patients presenting to the A&E with acute pain crisis
- Intravenous morphine (0.1 to 0.15 mg/kg), with reassessment of pain in 15 to 30 minutes after the dose is administered.
- Patients with severe pain may require repeated doses of intravenous morphine 0.02 to 0.05 mg/kg every 20 to 30 minutes to achieve pain relief.
- If adequate pain relief is achieved with a single dose, consider discharge to home on long-acting opioids with a prescription for medication for breakthrough pain.
- If the individual does not typically require long-acting opioids at home, discontinue the long-acting opioids when the pain event subsides.
- Hospitalization should be considered for around-the-clock parenteral analgesics if more than two doses of morphine or hydromorphone are required to control the pain episode.
Inpatient management of pain crisis
- IV opioids with a patient controlled Anaesthesia (PCA) should be considered as an initial option.
- For initial inpatient care in patients who are not taking opioids routinely, use intravenous morphine sulphate at 0.1 to 0.15 mg/kg every two hours or intravenous hydromorphone, 0.015 to 0.02 mg/kg IV every three hours. Reassessment is required 15 to 30 minutes after each dose is administered.
- When pain relief is not achieved with intermittent dosing of opioids, use continuous infusion of morphine or hydromorphone, preferably with a patient controlled analgesia (PCA) program that allows additional demand dosing.
- In the setting of significant renal or hepatic dysfunction, fentanyl is the IV opioid of choice.
- Use of benzodiazepines for insomnia should be avoided as they may predispose the patient to respiratory depression.
- Use of phenothiazines for nausea should be avoided as this may potentiate sedative effects. In the event that nausea is associated with opioid administration, odansetron is recommended as the antiemetic of choice.
- Ensure patients are well hydrated.
Variant sickle cell syndromes
There are several sickle cell variants linked to sickle cell gene in compound heterozygosity with other mutant beta globin genes. It is crucial that clinician do not assume the diagnosis but be mindful of these and carry out appropriate investigations to clinch the diagnosis. Especially in countries such as Maldives where significant number of cases of thalassemia still exist, the importance of this cannot be stressed enough. A summary of some of these are mentioned below.
1. Sickle beta+ thalassemia — Individuals with sickle-beta+ thalassemia have an illness that is less severe than HbSS disease. Disease severity is inversely related to the amount of HbA present, which varies from 5 to 30 percent. The peripheral smear shows the presence of hypochromic, microcytic red cells and levels of HbA2 are increased
2. Sickle beta0 thalassemia — Patients with sickle beta0 thalassemia have severe disease which may be somewhat less severe than HbSS disease. Unlike Sickle beta+ thelassemia no HbA is present on electrophoresis. It is distinguished from HbSS disease by the presence of hypochromic, microcytic red cells and increased levels of HbA2.
3. Sickle alpha thalassemia — The clinical manifestations and degree of anaemia in sickle alpha thalassemia are generally less severe than those seen in sickle beta0 thalassemia. HbA2 levels are increased according to the number of alpha globin gene deletions.
4. Sickle hereditary persistence of HbF (sickle HPFH) — Subjects with pancellular sickle HPFH are not anemic, do not suffer from vasoocclusive episodes, and may have HbF levels as high as 35 percent.
Conclusion:
The above description and treatment of the disease is not exhaustive . There are several other considerations to be mindful in managing the disease such as addressing the issue of pregnancy, treating prolonged and stuttering priapism, reducing the risk of stroke. Regular renal function and cardiovascular monitoring with renal and cardiac imaging should be carried out. Also addressing the issue of iron overload, vaccination, vitamin supplementation and treating infections are all very important aspects of their care. When appropriate all patients should be assessed for pulmonary hypertension.
Sickle cell disease is a multi system syndrome and carries with it a huge emotional and financial burden. As clinicians we are at the forefront of helping these, often very young lives who endure a great deal, every single day and for that reason it is crucial that these patients get the right diagnosis and the correct treatment at every stage of their care.
References
- Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. Jun 9 1994;330(23):1639-44.
- Gladwin MT, Sachdev V, Jison ML, Shizukuda Y, Plehn JF, Minter K, et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med. Feb 26 2004;350(9):886-9
- Pawliuk R, Westerman KA, Fabry ME, et al. Correction of sickle cell disease in transgenic mouse models by gene therapy. Science 2001; 294:2368.
- Mansilla-Soto J, Rivière I, Sadelain M. Genetic strategies for the treatment of sickle cell anaemia. Br J Haematol 2011.
- Wu LC, Sun CW, Ryan TM, et al. Correction of sickle cell disease by homologous recombination in embryonic stem cells. Blood 2006; 108:1183.
- Nienhuis AW. Development of gene therapy for blood disorders. Blood 2008; 111:4431.
- Perumbeti A, Higashimoto T, Urbinati F, et al. A novel human gamma-globin gene vector for genetic correction of sickle cell anemia in a humanized sickle mouse model: critical determinants for successful correction. Blood 2009; 114:1174.
- Zou J, Mali P, Huang X, et al. Site-specific gene correction of a point mutation in human iPS cells derived from an adult patient with sickle cell disease. Blood 2011; 118:4599.
- Wambebe C, Khamofu H, Momoh JA, et al. Double-blind, placebo-controlled, randomised cross-over clinical trial of NIPRISAN in patients with Sickle Cell Disorder. Phytomedicine 2001; 8:252.
- Cordeiro NJ, Oniyangi O. Phytomedicines (medicines derived from plants) for sickle cell disease. Cochrane Database Syst Rev 2004; :CD004448.
- Fawibe AE. Managing acute chest syndrome of sickle cell disease in an African setting. Trans R Soc Trop Med Hyg 2008; 102:526.
- Oniyangi O, Cohall DH. Phytomedicines (medicines derived from plants) for sickle cell disease. Cochrane Database Syst Rev 2010; :CD004448.
- Iyamu EW, Turner EA, Asakura T. In vitro effects of NIPRISAN (Nix-0699): a naturally occurring, potent antisickling agent. Br J Haematol 2002; 118:337.
- SINGER K, SINGER L, GOLDBERG SR. Studies on abnormal hemoglobins. XI. Sickle cell-thalassemia disease in the Negro; the significance of the S+A+F and S+A patterns obtained by hemoglobin analysis. Blood 1955; 10:405.
- SMITH EW, CONLEY CL. Clinical features of the genetic variants of sickle cell disease. Bull Johns Hopkins Hosp 1954; 94:289.
- Gonzalez-Redondo JM, Stoming TA, Lanclos KD, et al. Clinical and genetic heterogeneity in black patients with homozygous beta-thalassemia from the southeastern United States. Blood 1988; 72:1007.
- Gonzalez-Redondo JM, Kutlar A, Kutlar F, et al. Molecular characterization of Hb S(C) beta-thalassemia in American blacks. Am J Hematol 1991; 38:9.
Helenbeli Lounge
 It has been long discussed to provide a facility within the hospital for doctors to spend productive time during and or out of their duty hours. The “Helenbeli Lounge”, named after the prominent tamarind tree in the Hospital was recently opened exclusively for doctors. The name “Helenbeli” is the local name for tamarind.
It has been long discussed to provide a facility within the hospital for doctors to spend productive time during and or out of their duty hours. The “Helenbeli Lounge”, named after the prominent tamarind tree in the Hospital was recently opened exclusively for doctors. The name “Helenbeli” is the local name for tamarind.
The lounge is intended solely for doctors and provides a number of amenities for them. Equipped with workstations for research and work purposes, as well as a bookshelf with a number of medical books, doctors can spent time for research and academic development. Also, the lounge has a small pantry attached to it with amenities such as a fridge, microwave, electric kettle and other amenities.
 The aesthetics of the lounge makes it a really comfortable addition, which will positively impact on the doctors work environment.
The aesthetics of the lounge makes it a really comfortable addition, which will positively impact on the doctors work environment.
The longest serving doctor at the Hospital, Dr. RJC Pandian opened the lounge on 2nd July 2012. The Management hopes that the facility will be used productively to its optimal by all the doctors in the Hospital.
New COO and Interim CMO
We congratulate the new incoming top management staff to the Hospital and with them the best of luck in their new appointments.
Mr. Abdulla Shinah was appointed as the COO of ADK Hospital on June 27, 2012. Mr. Shinah has extensive management experience in the Maldives, both in the healthcare and non-healthcare settings. His appointment follows the departure of the previous COO, Dr. Ahmed Jamsheed Mohamed. The management thanks him for his very productive services in a short tenure.
On July 1, 2012, the Management appointed Dr. Mijares, Consultant ENT as an interim CMO. Dr Mijares will fill in the post till a permanent CMO is appointed. With the intended departure of the previous CMO, Dr. Nitin, this arrangement is transitional.
The Management is fully confident in the capacity of these two gentlemen in fulfilling the task assigned them with these appointments. Management is also confident that all staff will continue to support the COO and CMO in discharging their duties.
ބޭސްވެރިކަމުގެ އިންގިލާބު: އިބްނި ސީނާގެ ބޭސްވެރިކަމުގެ ގާނޫނު
– މުޙަންމަދު ޒާހިރު ހުސައިން –
ބޭސްވެރިކަމުގެ ސައެންސަކީ ޒަމާނާއެކު އެންމެ ބޮޑު ބަދަލުތަކެއް އައިސްފައިވާ އޭރިޔާ އެކެވެ. އޭގެ ބަދަލުތައް އައީ އަކީ ހަމައެކަނި ގުޅަ ބޭހާއި އިންޖެކްޝަނާއި ހަށިގަނޑު ފަޅާހެދުމުގެ ކަންކަމަށް އެކަންޏެއް ނޫނެވެ. އޭގައި ގެންގުޅޭ އާލަތްތަކާއި ސާމާނުތަކަށް ވެސްމެއެވެ. ފަޅާ ހެދުމުގެ މަސައްކަތުގަެ ވަގުތުތައްވެސް ޒަމާނާއެކު ވަރަށް ބޮޑުތަން ތަފާތުވެފައި ވެއެވ.ެ
 ބޭސްވެރިކަމުގެ ތާރީޚަށް ބަލާއިރު އެކަމަކީ ވަކި ޒަމާނެއްގެ ވަކި ބަޔަކަށް ނިސްބަތްވާ ކަމެއް ކަމުގައި ކަނޑައަޅާ ބުނެވޭކަށް ނެތެވެ. އިނގޭ އެއްޗަކީ އިންސާނުން ދުނިޔެ މަތީގައި ލެއްވުވީއްސުރެ އެބައިމީހުންނަށް ދިމާވާ އެކިއެކި ކަންކަމަށް އެ ޒަމާނަކަށް އެކަށިގެންވާ ހައްލުތައް ހޫދަމުން ގޮސްފައިވާ ކަމެވެ. މިގޮތުން އެބައިމީހުންނަށް ޖެހޭ ބަލިތަކަށް ހައްލު ހޯދުމަށް އެ ޒަމާނަކާ އެކަށީގެންވާ ކަންތައްތަކެއް ކޮށްފައިވާކަން ތާރީޚުން ކޮންމެވެސް ވަރަކަށް އެނގެއެވެ. މިގޮތުން އެބައިމީހުންގެ ވެށީގައިވާ ގަސްގަހާހެހީގެ ފަތްޕިލާވެއްޔާއި އަދި ބިމުގެ ބައެއް މައުދަނު ނުވަތަ ގަލާއި ހިލަވެސް ބޭނުންކޮށްފައިވާކަން އެނގެއެވެ. އަދި މިކަންކަމުގެ އިތުރުން ފަންޑިތަ އާއި ހާހޫރައިގެ ބޭނުން ކޮށްފައި ވެސް ވެއެވެ.
ބޭސްވެރިކަމުގެ ތާރީޚަށް ބަލާއިރު އެކަމަކީ ވަކި ޒަމާނެއްގެ ވަކި ބަޔަކަށް ނިސްބަތްވާ ކަމެއް ކަމުގައި ކަނޑައަޅާ ބުނެވޭކަށް ނެތެވެ. އިނގޭ އެއްޗަކީ އިންސާނުން ދުނިޔެ މަތީގައި ލެއްވުވީއްސުރެ އެބައިމީހުންނަށް ދިމާވާ އެކިއެކި ކަންކަމަށް އެ ޒަމާނަކަށް އެކަށިގެންވާ ހައްލުތައް ހޫދަމުން ގޮސްފައިވާ ކަމެވެ. މިގޮތުން އެބައިމީހުންނަށް ޖެހޭ ބަލިތަކަށް ހައްލު ހޯދުމަށް އެ ޒަމާނަކާ އެކަށީގެންވާ ކަންތައްތަކެއް ކޮށްފައިވާކަން ތާރީޚުން ކޮންމެވެސް ވަރަކަށް އެނގެއެވެ. މިގޮތުން އެބައިމީހުންގެ ވެށީގައިވާ ގަސްގަހާހެހީގެ ފަތްޕިލާވެއްޔާއި އަދި ބިމުގެ ބައެއް މައުދަނު ނުވަތަ ގަލާއި ހިލަވެސް ބޭނުންކޮށްފައިވާކަން އެނގެއެވެ. އަދި މިކަންކަމުގެ އިތުރުން ފަންޑިތަ އާއި ހާހޫރައިގެ ބޭނުން ކޮށްފައި ވެސް ވެއެވެ.
ރެކޯޑް ކުރެވިފައިވާ ބޭސްވެރިކަން:
އިންސާނީ ހަޟާރަތްތަކުގައި ބޭސްވެރިކަމުގެ ރިކޯޑް އެންމެ ފުޅާކަންމަތީ އޮތް އެއްބަޔަކީ ކުރީގެ ގްރީކް މީހުންގެ މެދުގަ އެވެ. އެއަށް ދިވެހިން މިކިޔަނީ ހަކީމީ ބޭސްވެރިކަން ނުވަތަ ޔޫނާނީ ބޭސްވެރިކަމެވެ. ހަމަ އެފަދައިން ޗައިނާ އާއި މިސްރުގެ ހަޟާރަތުގައި ވެސް ބޭސްވެރިކަމުގެ ރެކޯޑް އޮތް ކަމުގައި ވެއެވެ.
ކޮންމެއަކަސް ލިޔެވިގެންވާ ރިކޯޑް އެންމެ ބޮޑަށް ފާހަގަ ކުރެވެނީ ކުރީގެ ގްރީކް މީހުންގެ މެދުގައެވެ. އެބައި މީހުންގެ މެދުގައި ސައެންސާ ފަލްސަފާ ކުރިއަރައި ދިޔަ ޒަމާނުގައެވެ. އެބައި މީހުންގެ ސައެންސްވެރިން ނުވަތަ ހަކީމުންގެ ޒަމާނުގައެވެ. އެ ޒަމާނުގައި ސައެންސާއި ފަލްސަފާ އޮތީ މުޅިން އެހެން ނާރެހެއްގެ ގޮތުގައި ހުރިހާ ސައެންސަކާ ޢިލްމެއް އެކައްޗެއްގެ ގޮތުގައެވެ. ގްރީކް ފަލްސަފާ ވެރިންނަކީ ހަކީމުންނެވެ. އެހެންކަމުން އެއީ ހަކީމީ ބޭސްވެރިކަން ކަމުގައި ދިވެހިން ގެ މެދުގައި ނަންކުރެވިގެން އައިސްފައިވަނީ ކަމުގައި ބެލެވިދާނެއެވެ. ހުރިހާ ސައެންސަކާ އިލްމު އެކުލެވިފައިވާ ނާރެހެއްގެ ގޮތުގައި މާނަކޮށް ދިނުމުގެ ގޮތުންނެވެ. ބޭސްވެރިކަންވެސް އެޒަމާނުގައި އެއީ ފަލްސަފާގެ ނާރެހެވެ. ފަލަކު އިލްމާއި ހިސާބު އިލްމު ވެސް އެއީ ހަމަ ފަލްސަފާވެރިންގެ ނާރެހެވެ.
ގްރީކް ފަލްސަފާގެ ޒަމާނުގައި އޮތް ބޭސްވެރިކަމުގެ ބޭހުގެ ދާއިރާގައި ފަތްޕިލާވެލީގެ ތައުސީރުތަކާއި އޭގެ ފައިދާގެ މައްޗަށް މުސްލިމުންގެ ފައިލަސޫފު އިބްނިސީނާ ލިޔުއްވި ބޭސްވެރިކަމުގެ ގާނޫނަކީ މުސްލިމުންގެ ތެރެއަށް މިދާއިރާގައި އެޒަމާނުގައި އައި ބޮޑު އިންގިލާބެއް ކަމުގައި ބެލެވެއެވެ. އެފޮތުގައި ތަފާތު ފަތްޕިލާވެއްޔާ ގަސްގަހުގެ ފަތާއި މުލުގެ ފައިދާތަކާމެދު ވަރަށް ސާފުކޮށް ލިޔުއްވާފައި ވެއެވެ. އަދި އޭގެ ތަޖުރިބާތަކާއި އެކަމުން ތަފާތު ބަލިތައް ފަސޭހަވުމާއި އެތަކެތި ބޭނުން ކުރަންވީ މިންވަރު ހާމަކުރައްވާފައި ވެއެވެ. އޭގެ ތަފާތު އެތަކެއް މިސާލުތައް އެފޮތުގައި ވެއެވެ. ފައިދާ އާއި ގެއްލުމާއި ތަފާތު ބަލިތަކަށް އޭގެ އަސަރު ކުރާނޭ ގޮތުގެ ވާހަކަތަކެވެ.
– ދެވަނަބައި އޯގަސްޓް 2012 ގެ އަދަދުގައި –
The time factor: my doctor is in a hurry!
Many a time when we go and see a doctor, there is a feeling that the doctor is in a hurry or rushed, distracted or doesn’t really care about the patient. Health systems are increasingly facing the issue of inadequate time being given to patients by doctors. It is a global phenomenon. Proper interactions between the patient and the doctor are an integral part of medical care. Research shows that outcomes of medical care are more successful when a trust is gained between the patient and doctor through spending adequate time and understanding the life and health of the patient.
 Ironically, at present many of the doctors do not give adequate amount of time to the patients. In our efforts to improve patient care, we developed and implemented a Code of Professional Conduct for clinicians at ADK Hospital. In the Maldives, this is the first such initiative taken by a healthcare provider. One of the key factors of the Code is to spend enough time with the patients. Subsequent protocols of the hospital also reiterate this matter since if the Code and the Protocols are to be adhered, a significant change in the time spent with patient should happen. A change in a culture is always a challenge.
Ironically, at present many of the doctors do not give adequate amount of time to the patients. In our efforts to improve patient care, we developed and implemented a Code of Professional Conduct for clinicians at ADK Hospital. In the Maldives, this is the first such initiative taken by a healthcare provider. One of the key factors of the Code is to spend enough time with the patients. Subsequent protocols of the hospital also reiterate this matter since if the Code and the Protocols are to be adhered, a significant change in the time spent with patient should happen. A change in a culture is always a challenge.
We conducted an audit at doctors’ OPD’s to determine the amount of time doctors spend with patients. Given that the doctors have to take a patient history, examine the patient, write the records and produce a prescription, obviously time is needed to ensure all these are done. In most cases the average time spent per patient is 5 minutes or less for the departments that the audit was conducted. This is a very little amount of time spent on patient care. Efforts need to be put into to ensure that this is changed. Continuous monitoring and making doctors to understand the importance of the time factor is crucial. In fact, it is the doctors who gain from a little change in their current habits.
There are many reasons why this change needs to occur. It should occur across the whole health system in the Maldives as well. For example, the time factor contributes to
Patient satisfaction. Patient’s who visit doctors who spend more time and involve patient in care are seen to be more satisfied with the care that they got and are less likely to leave that practice of that doctor.
Outcome of diseases. Although no concrete evidence is shown in research, there are some research findings that indicate that longer consultations have lead to more understanding of the disease by the patient and hence lead to better outcomes.
Rational prescribing. Studies have shown that shorter consultations have longer prescriptions. Doctors who spend more time with patients are shown to prescribe medication and investigations more rationally than those who spend less time.
Doctor satisfaction. There is ample research that shows longer visit lengths foster better patient interactions that lead to better satisfaction for doctors. In fact, studies show that good patient relationships increase doctor’s confidence and satisfaction and hence lead to better quality of care as well.
Lower risk of malpractice/negligence claims. It is also seen that doctors who tend to have better patient relationships, given the above factors as well, have found to be less likely to face malpractice and or negligence charges.
So what is the ideal amount of time a doctor should spend with the patient on a visit? There is no concrete evidence as to what it the optimal time for a doctor’s visit. What is seen is that longer visits allow time for more attention to many aspects of care. Patient participation and education increases thus leading to better outcomes.
For us, understanding this aspect of care and adhering to existing protocols and standards addressing the issue will be a start towards an improved quality of care.
International World No Tobacco Day 2012 – Feature Article
– by: Dr. Aishath Aroona Abdulla, Maldives Medical Association –
Tobacco Industry Interference with Promoting Good Health
On 31 May every year, the world commemorates World No Tobacco Day. This day has been set apart to give an opportunity to educate people worldwide and to help nations to focus on interventions for tobacco control, because tobacco is an extremely hazardous and highly addictive substance, causing a great deal of death and suffering, and needs special collective efforts by a multitude of groups and individuals to control its use and consequences.
Tobacco was introduced to the world after Christopher Columbus landed in America in 1492. It was since transported to other countries across the world and within 150 years, has become a major trade commodity with a huge market internationally.
Tobacco is a major health hazard, causing 6 million deaths worldwide every year. 600,000 of these are non-smokers exposed to second-hand smoke. Tobacco kills one in every two users of tobacco, and it kills slowly, bringing much suffering – physical, mental and social – over several years before finally killing. Scientific research has proven that tobacco causes many illnesses involving almost all the different systems in the body, and affect people of all ages, particularly children and pregnant women. Some common illnesses include stroke, heart attacks and many illnesses of the respiratory system that become irreversible later in adults, in addition to lung cancer and many other types of cancer. Second-hand smoke causes asthma, pneumonias and many other respiratory illnesses in children. Exposure to tobacco smoke in pregnancy causes abortions, premature delivery, small for gestation babies and can lead to sudden infant deaths (SIDS). Newer research also suggests that exposure to tobacco smoke in early life may be associated with certain disorders of brain development. And no benefits have been shown to-date despite extensive research. In Maldives, it is estimated that tobacco accounts for more than a quarter of deaths. Thus tobacco is a hazardous substance that should be strictly controlled.

Tom And Jerry Slapped With Smoking Ban. by Stuart Heritage on August 22, 2006 http://www.hecklerspray.com/tom-and-jerry-slapped-with-smoking-ban/20064524.php
If tobacco were not harmful to health there would be no reason to control its use. Four cigarette manufacturers dominate about three-quarters of the global market. These are very wealthy, trans-national companies, thus yielding immense power, above that of individual nations. Tobacco companies work for profit. They resort to various devious tactics to increase their sales.
- Tobacco industry targets low and middle income countries–
- Many developed countries have now made strong laws that prohibit smoking in public places, prohibit advertising, restrict production, import, sales, and tax tobacco heavily. These are proven methods to reduce tobacco consumption and thus the harm. Tobacco industry knows they cannot sell in these countries, and so specifically target low and middle income countries which have poor laws and low education among their population. Nearly 80% of the world’s one billion smokers live in low- and middle-income countries
- Tobacco industry targets children– tobacco companies know that tobacco causes premature deaths. So they want to recruit more smokers to make up for the loss from premature deaths. They specifically target children by interfering with laws, specific advertisement and promotion in films.
- In the United States, 390,000 kids are recruited to smoke each year by the smoking they see on screen, worth $4 billion in lifetime sales to the tobacco companies.
- Do your kids see smoking in movies in Maldives?
- Check the cartoons – e.g.
- Check the cable TV channels – they may not be regulated under our laws.
- Movies from the internet (e.g. YouTube) are not regulated at all. Many teenagers in Male’ watch films off YouTube.
Tobacco companies target the youngest children possible. Younger the child, the more lasting the impression, the higher chances of taking up smoking, and the harder to quit.
- Tobacco industry targets women– “women are vulnerable” they say. Actually, they know that if a mother smokes, it increases the chances that her children will smoke , creating a whole family and generation of smokers. They specially advertise to women since post-world war 1920’s, when they deceived women into associating cigarettes with women’s rights.
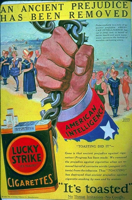
- In 1929 – a tobacco company hired Edward Bernays (named by some as the father of public relations) to stage a parade in New York City, showing models holding lit Lucky Strike cigarettes, that they called “Torches of Freedom“. Women immediately associated it with women’s rights, and smoking increased among women. Today, many women still think it is a woman’s right to smoke, while tobacco slowly kills more women.
- In modern times, tobacco industry advertises that cigarettes help loose weight, showing models with slim figures, while in reality, smokers lose their appetite, and become thin and wasted.
- New types of cigarettes like “Lights”, flavoured cigarettes (mint, strawberry, etc. are specially targeted for teenage girls.
- (“Lights” are a misnomer. They claim to have low tar, but actually have low nicotine, that makes people smoke more cigarettes and spend more of their money, while exposing themselves to the same risk or higher, of getting ill.)
- Tobacco industry advertises in devious, indirect ways
- Movies – they use a method called “product placement”. Film-makers are paid to add scenes where main characters are shown to smoke in various situations, and can be depicted as rebellious, fun, stress-relieving, the list goes on. Brands are often displayed in the film. This is an underhand way of sending messages to the unsuspecting brain, where people don’t realize that they are seeing an advertisement. Big Tobacco pays actors, actresses and producers to get their products into the movies.
- Using role models to entice young adolescents to smoke – e.g. actors smoking off-screen, paid models smoking in places young people frequent, like shopping malls, supplying free cigarettes to film-stars and armed forces officers to entice young boys to smoke, etc., especially where advertising is restricted.
- Philanthropy – They sponsor sports, arts charity events, etc. to get sympathy and “show people they do good”, while they kill millions of people worldwide (estimated 600 million deaths per year)
-
- Tobacco industry distorts scientific research – As scientific research increasingly proved that many illnesses, like lung cancer, and an extensive list of other illnesses are caused by tobacco, the industry hired scientists to write to journals and lay media questioning these research, and stating that these findings are doubtful. This helps to keep their consumers. People continue to not worry about smoking when they are not sure if it causes illness. Many diseases are actually proven to be caused by tobacco, several by good scientific research studies with large numbers of participants and good study methodology.
- Tobacco industry lobbies politiciansand political parties in most countries. – They do this to prevent good laws, make loopholes for them, so that they can continue to “do business”. They make monetary deals, bribe, fund election campaigns, and even send false “experts” to give unsuspecting governments advise against making solid tobacco control laws.
- Joint manufacturing agreements: Tobacco companies form joint ventures with state monopolies and subsequently pressurize governments to privatize monopolies
- Creating Smokers’ rights groups: Tobacco industry make an issue and create their own supportive groups to create an impression of spontaneous, grass-roots public support. These include: Smokers’ rights groups, women’s rights groups, tobacco farmer’s groups, tobacco company workers’ groups, tobacco seller’s groups, and even so-called “consumer groups”. These are fake groups. Tobacco companies bring out issues as if they affect these people severely, and make the people gather together to “stand up for themselves”, while they actually fight to make the companies richer.
- Intelligence-gathering: Tobacco industry carries out regular market study and researches on how they can create demand by influencing how people think to promote their products. Thus they are often ahead of public health authorities.
- International treaties: Tobacco industry uses international trade agreements to force entry into closed markets and limit countries ?form increasing taxes. Now, however, the World Bank no longer supports tobacco industry (including tobacco farming) with any type of funding or concessions.
- Intimidation: They use legal and economic power as a means of harassing and frightening opponents. They have filed court cases in countries that introduced smoke-free laws, e.g. India
 How did this information come out?
How did this information come out? In earlier days, tobacco companies would openly advertise that their brand did not bring cough, or were safer, etc. As people who got cancer learned from doctors and medical evidence that tobacco cause lung cancer, they sued the tobacco companies for lying. That is how many of these company secrets leaked out. Today, health authorities follow them stringently and try to identify their strategies. Still tobacco companies are ahead, because they have wealth and power, and conduct regular market research.
The solution:
Tobacco is difficult to control due to its addictive nature, and due to the influence from tobacco industry. Therefore the World Health Organization (WHO) established a special Tobacco-Free Initiative in May 2003, to focus on tobacco control, and prepared a treaty called the Framework Convention for Tobacco Control (FCTC) which came into effect in February 2005. WHO FCTC recommends a package including multiple methods of control, named the MPOWER package. To-date, 174 countries including Maldives are signatories to the FCTC. By signing, a country agrees to commit towards tobacco control by establishing the strategies of the MPOWER package.
All these methods are proven to be effective. However, the size of effect of a single intervention is relatively small, therefore WHO recommends that all these interventions be used in combination to control tobacco and tobacco-related disease effectively.
So it is important that we as a nation carry out all these methods to prevent harm from tobacco in Maodives. Act now.
Towards a Tobacco-Free Maldives.
New Wheelies …
 It is not very often that we look at how new technology and innovations may matter in very small things that matter. Given the complexity of a hospital’s operation, one would think that a wheel chair is a very simple matter. However, modern technology has been in full force to make modern wonders in all aspects of patient care. Of course as our visions states, to be the leading healthcare provider in the country through innovation and excellence, ADK Hospital also looks at such developments closely and tries to implement modern technology.
It is not very often that we look at how new technology and innovations may matter in very small things that matter. Given the complexity of a hospital’s operation, one would think that a wheel chair is a very simple matter. However, modern technology has been in full force to make modern wonders in all aspects of patient care. Of course as our visions states, to be the leading healthcare provider in the country through innovation and excellence, ADK Hospital also looks at such developments closely and tries to implement modern technology.
This new wheel chair is far from what is seen. Many people have curiously looked at the new wheel chairs at ADK Hospital. These wheel chairs are state of the art innovations for modern hospitals. This wheelie is known as the Space Saver and sets new standards for quality and functionality. This new product provides patient transfer in an easy and comfortable way both to patient and the caregiver.
Hospitals, with all the crowd and “traffic” in it, resemble the disorder of cities. In order to minimize this chaotic situation and make the environment tidier, the park station makes it really convenient when in need for space.
Patients are already feeling the ease and comfort of the chair with positive feedback to the Hospital. We hope that little things that matter can be improved in future too and make the patient more comfortable while in the care of our team.
World blood donor day
Every year, June 14 is marked as world blood donor day. According to the World Health Organization, June 14 is marked as the day to recognize the millions of people who save lives and improve the health of others by donating blood. The Day highlights the need to regularly give blood to prevent shortages in hospitals and clinics, particularly in developing countries where quantities are very limited.
 In the Maldives, there is a very high need for blood donation and requires major public awareness on blood donation. This year the theme is ‘every donor is a hero”. Rightly so, we donate blood to save lives. With an endemic thalasaemia situation and more than half of the pregnant women in the country being anaemic, the need and the potential need for blood is very high.
In the Maldives, there is a very high need for blood donation and requires major public awareness on blood donation. This year the theme is ‘every donor is a hero”. Rightly so, we donate blood to save lives. With an endemic thalasaemia situation and more than half of the pregnant women in the country being anaemic, the need and the potential need for blood is very high.
Despite the need, there are many challenges. Firstly willing donors are scarce. Perhaps myths associated with donation. Major awareness creation is needed.
Secondly banking facilities are scarce too. To be exact, national banking still has issues and is highly limited. Especially for islands the situation is extremely bleak. Hence, it is imperative that such issues are addressed.
ADK Hospital also puts some effort to introduce blood banking. At present major equipment is installed and training is ongoing. It is envisaged that the blood bank will be in full swing by end of July.
To celebrate the blood donors day, the hospital ran a donor registration and awareness creation clinic for the day. Although it was not a major attraction, considerable achievements were made to collect potential donors for the proposed blood bank.
I’m a doctor. Must you trust me?
The doctor-patient relationship is one that is grounded on trust. There is a tacit belief in the doctor’s goodwill and competence, resulting from an imbalance of power between the patient and doctor in terms of knowledge. And where there is ignorance, and uncertainty, trust is a must. The lack of knowledge seems crucial to the notion of trust. Even where knowledge is possible, as when the patient is a doctor himself, he must feign ignorance, because trust is described as one of the virtues of being a good patient, together with truthfulness, justice, and probity. Trust is required because medical care depends upon judgement calls that are not predictable, and the good patient is one who recognizes this. A doctor is not allowed to treat himself as his judgement is deemed clouded when sick, and he must submit to the treatment of other doctors and pretend not to be certain of outcomes. The struggle here is obvious, and it is not surprising that doctors qua doctors turn out to be the worst of patients.





You must be logged in to post a comment.